Declaration of CTCA-Founders
Josef Hummelsberger, Axel Wiebrecht, Stefan Kirchhoff, Ingolf Hosbach, Karin Bervoets-Fauska, Reinhard Rapp
Every doctor or therapist who works with Chinese medicines and applies and prescribes them must take a critical look at their quality, identity and purity as well as possible side effects of these.
In Germany, Switzerland and Austria, mainly the pharmacists, wholesalers and supervisory boards are responsible for safeguarding the quality of these drugs. Quality, identity and purity of crude drugs have to be checked by all parties and must be certified. However, side effects or adverse effects (AEs) of the drugs themselves are another matter. The prescribers are responsible for these, and their responsibilities include knowing about possible contraindications and side effects, taking of appropriate precautionary measures (e.g. obtaining laboratory values), recognizing and correctly interpreting any side effects and, finally, reacting appropriately.
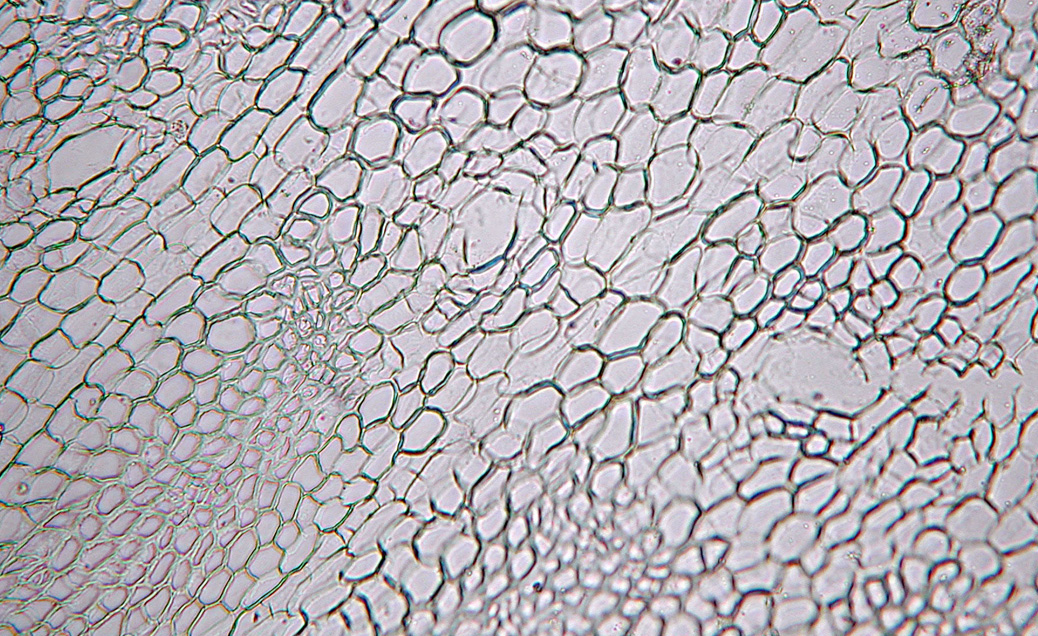
Chinese Herbal Therapy (CHT) is an allopathic medicinal tradition. The medicinal ingredients and their interactions with the human body achieve its pharmacological effects.
Several side effects are already known or may occur:
Allergic reactions:
These are generally possible with all substances, including foodstuffs. With regards to CHT, the authors have noticed occasional allergic reactions after ingestion of Menthae arvensis herba (bohe), Chrysanthemi flores (juhua) and Paeoniae lactiflorae radix (baishao).
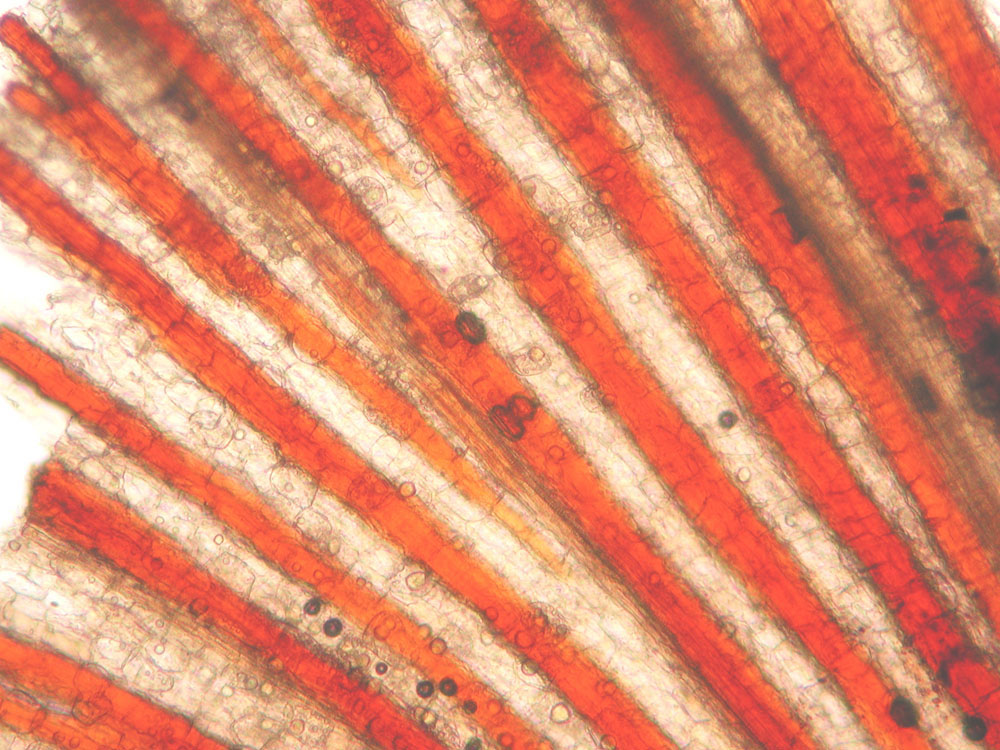
Hepatotoxicity:
Several publications (1,2) have reported raised liver enzymes caused by traditional Chinese decoctions or prepared medications. Melchart et. al. only found minimal and reversible increases of transaminases. Their overall calculation even showed a decrease in the liver enzymes values. With high doses and pre-existing hepatic diseases, a disturbance of liver function became more likely (2). Cases of severe hepatic failures have also been reported, although in these cases, there were indications that they were caused by immunological reactions (3).
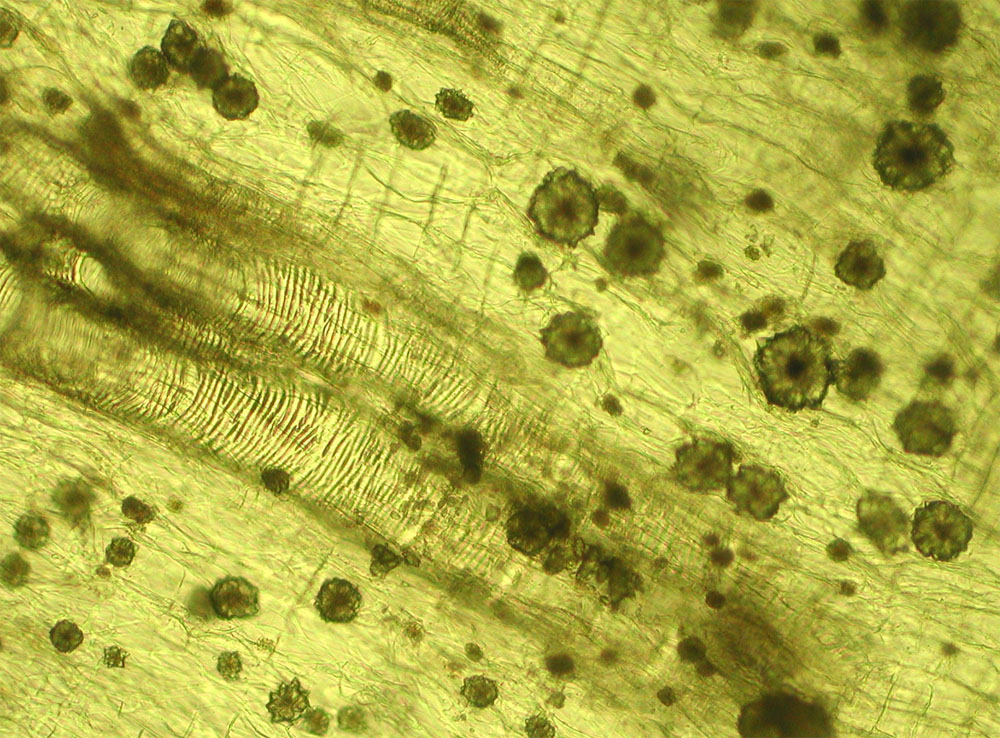
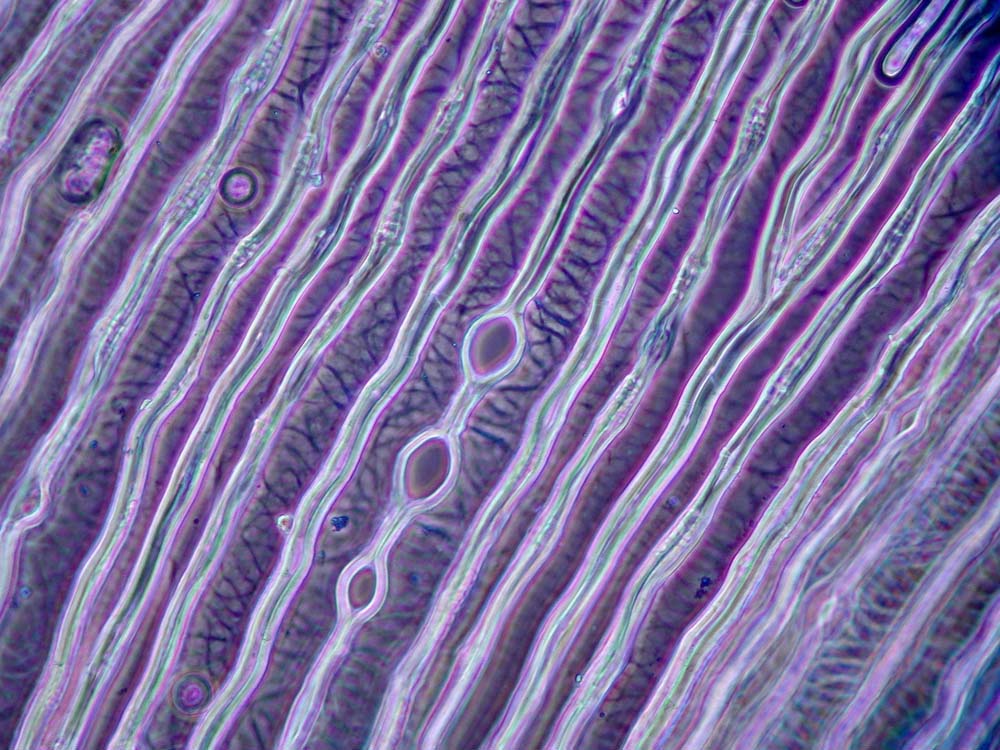
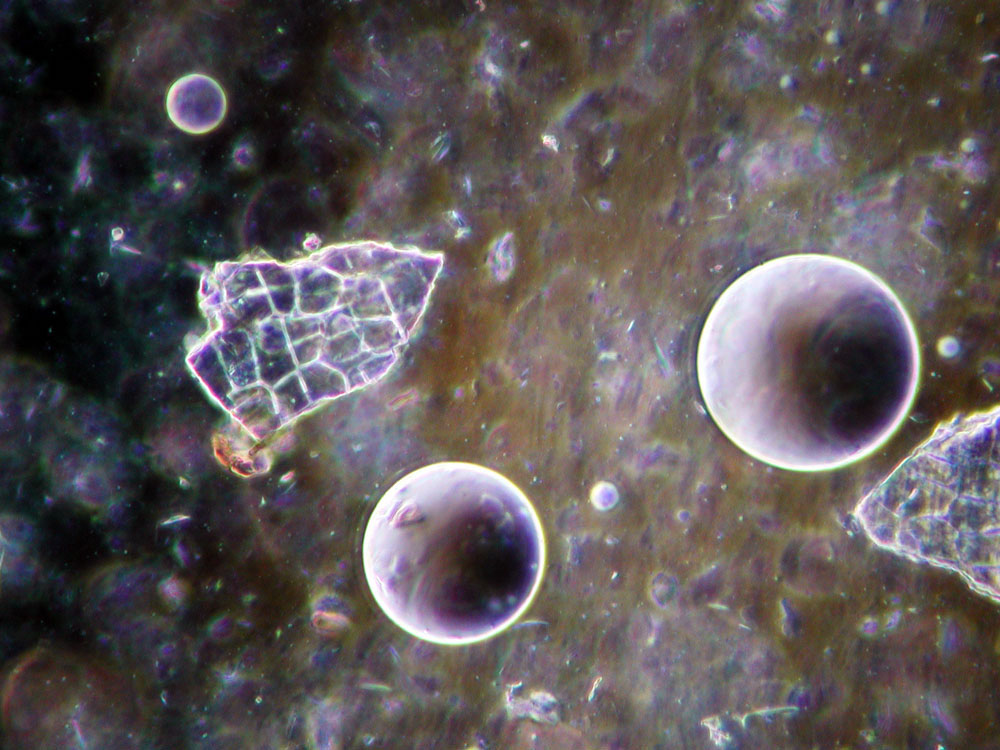
Nephrotoxicity:
There are several documented cases of dose-dependent nephrotoxicity and teratogenicity of aristolochic acid (4,5,6,7). Medical drugs, which can be confused with plants containing aristolochic acid (e.g. Clematis seu akebiae caulis, mutong), therefore have to be examined for aristolochic acids before they are delivered to pharmacies. Nevertheless, two years ago, a case of acute renal failure occurred when an American patient living in Germany took a patent remedy to treat his prostate disease (8).
Synergistic effects with other medications:
A huge number of Chinese medical drugs are metabolized by the liver. If the cytochrome P450 system -which is genetically polymorphic and has a limited capacity- is already overloaded by other pharmaceuticals, this may result in either a faster or slower metabolism of Chinese drugs. The lessons learnt from prescribing kava-kava have shown that in many cases of hepatotoxicity, biomedical drugs which also cause liver damage, such as contraceptives, were also responsible, or there was a concurrent alcohol intake.
Special attention has to be paid to oral anticoagulants whose metabolism or blood protein binding may be affected by Salviae radix (danshen) or Angelicae sinensis radix (danggui), leading to dangerous blood coagulation disorders (9).
Side Effects caused by non-observance of contraindications:
Several Chinese drugs carry known risks, which must be carefully observed. Ephedrae herba (mahuang), Ginseng radix (renshen) and also Glycyrrhizae uralensis radix (gancao) may increase blood pressure if taken in higher doses. Special attention has to be drawn to contraindications in pregnancy as they are listed in the Chinese Materia Medica as well as those which have been emerged in the latest perception.
Side effects caused by incorrect treatment:
A faulty diagnosis and subsequent erroneous treatment strategy may intensify existing clinical symptoms or cause new symptoms. This phenomenon is known among to all TCM-therapists. B. Kirschbaum illustrates this point with an impressive case study in (10).
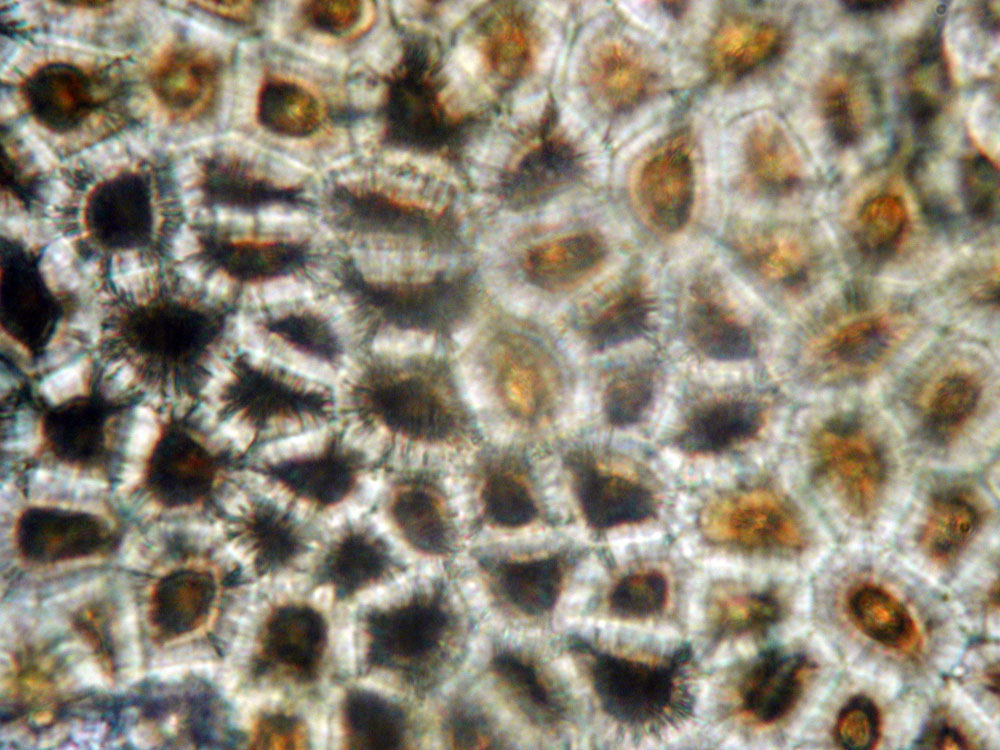
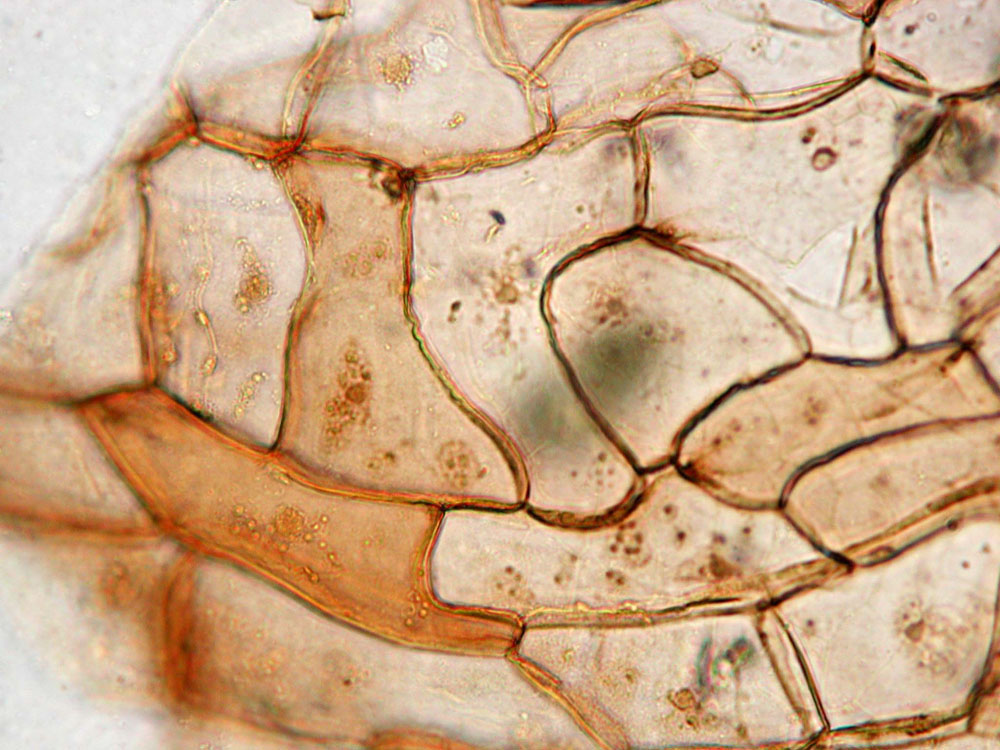
Side effects caused by mistaken identity, contamination or undeclared additives:
Several international articles have reported that patent remedies - especially those from China - in some measure contain undeclared added components such as cortisone, sildenafil, diclofenac, etc. (11) for which a fraudulent intention must be assumed. Fortunately, in Germany this problem is of lesser concern due to the strict rules governing pharmacies and to the responsible quality controls on the part of the pharmacists. However, this safety net is undermined by the increase of offers for CHT preparations via online pharmacies. This risk may be avoided by the usage of crude herbs, but the problem of identification remains. The latter can be avoided by using only certified, specialized pharmacies such as those belonging to the Arbeitsgemeinschaft Deutscher TCM-Apotheken (Working Group of German TCM-Pharmacies).
In our summary, we have attempted to show that CHT- although rarely - may cause significant side effects. Although many of the drugs have been used for millennia, the documentation and recognition of side effects in ancient and modern China were and remain fragmentary and unreliable. An example of this is mutong; although there had been incidents of severe and also deadly intoxications with Aristolochia in China (12), no adequate reaction on the part of the medical community or the Chinese authorities has yet taken place.
Some of these problems may well lead to a medical or legal situation, which is beyond the competence of most therapists. Collection of data, dissemination and strict observance of the existing knowledge about risks can help prevent AEs. If and when organ damage is observed, this is frequently and all-too-rapidly attributed to the administration of naturopathic remedies; an example of this is the (German) Federal Drug And Medical Devices Institute's (BfArM) reaction in the case of kava-kava. The efficacy of natural remedies is considered unproven in a scientific way, and this argument is frequently used to immediately remove these remedies at the first suspicion of side-effects. A later analysis of the reported cases of hepatic failure following the consumption of kava-kava showed that of 19 reported cases, only one could be likely and another one possibly associated with the use of the drug (13). The European Pharmaceutical Board EMEA will issue monographs concerning traditional medical drugs of every provenance in the near future, an essential requirement of which will be therapy safety.
Because of this, several societies and individuals (among them Annette Wrobel, AGTCM; Josef Hummelsberger, SMS; Stefan Kirchhoff, DWGTCM/University Witten-Herdecke; and Anna-Regina Flechtner, TCM-Apo AG) have joined together following the initiative of Axel Wiebrecht (DÃGfA) and founded the Centre for Safety Chinese Herbal Therapy (CTCA). The CTCA welcomes the cooperation of all serious practitioners and instructors of CHT. The German Chinese medical societies (SMS, DÃGfA, AGTCM, DWGTCM, DECA) are financially supporting this centre as far as possible. The work will initially be taken over by a council, which is made up of representatives from the participating societies and expert advisors, among them pharmacists. One medium-term goal of the CTCA is to establish ties with universities. Further objectives include:
Reporting and evaluating side effects:
We ask all practitioners of CHT to report to the representative of her/his society any suspected case of side effects by means of the registration form. These reports - which will be kept in strict confidentiality - will be used to investigate the case and to determine whether CHT is the culprit for these side effects. The following registration form was designed for this task. Bearing in mind the often large numbers of prescribed ingredients, only accurate and detailed data will make it possible to draw conclusions about causal interrelations. In your own interest, we ask you for your cooperation.
Reporting verified AEs: In order to further improve therapy safety, any verified information about AEs will be published in the subject-related publications and be transmitted to the societies and instructors following a detailed evaluation by the council. A therapist can only avoid adverse effects if individual reports are evaluated and the findings made available to him.
Rejecting unjustified accusations against CHT: In the event of undesired medical effects, identifying the causes can be difficult to verify. With the help of an extensive differential diagnosis, which should take place shortly after the AE was observed, the suspicion falling on CHT can be either specified or eliminated . This is often impossible at a later time. For example, if hepatic enzymes are elevated, many other possible reasons have to be excluded (e.g. in the case of an acute EBV infection. A later distinction between an acute or past infection is impossible in many cases). Western medical practitioners, government officials and the press tend to blame CHT for reactions that cannot be clearly attributed to other causes. In Belgium, CHT was held responsible for heart valve defects that later turned out to have been caused by appetite depressants (7). A detailed documentation of reported cases can often help eliminate a connection to CHT.
Recruiting experts to help draw up CHT-monographs: The CTCA strives to secure the therapists' influence and the availability of the drugs with a positive risk benefit ratio by assisting with the writing of the EU monographs. The drawing-up of these monographs must not be left solely to the authorities and toxicologists. The point of view and expertise of CHT practitioners is essential.
International cooperation: The centre's medium-term goal is cooperation in the field of therapy safety with similar initiatives from other countries. These exist in Australia, Belgium and Switzerland, among others. Cooperating with organizations in German-speaking countries is a priority.
Using the Centre's expertise in planning research studies: The CTCA's long-term goal is to build up a reputation in order to help with the planning of research studies on CHT. The centre's team will offer their expertise for such plans.
Improving communication: The CTCA hopes to initiate a lively professional and scientific discussion and intercommunication between all CHT societies.
Names and addresses of the participating societies and institutions:
| AGTCM | (Arbeitsgemeinschaft für klassische Akupunktur und Traditionelle chinesische Medizin): Dr. Karin Bervoets-Fauska, Rotlintstr. 68 H, 60316 Frankfurt, telefax: 00-49-69-43-05-77-73, |
| DÄGfA | (Deutsche Ãrztegesellschaft für Akupunktur): Dr. Axel Wiebrecht, Bundesallee 141, 12161 Berlin, telefax 00-49-30-82-70-42-64, |
| DECA | (Gesellschaft für die Dokumentation von Erfahrungsmaterial der Chinesischen Arzneitherapie): Dr. Reinhard Rapp, Seelbergstr. 16, 70372 Stuttgart, telefax 00-49-711-55-16-44, |
| DWGTCM | (Deutsche Wissenschaftliche Gesellschaft für Traditionelle Chinesische Medizin): Dr. Ingolf Hosbach, Dr.-C.-Otto-Str. 129, 44879 Bochum, |
| SMS | (Societas Medicinae Sinensis): (formerly Dr. Josef Hummelsberger, at present:) Dr. Christian Thede, Gorch-Fock-Weg 16, 23730 Neustadt in Holstein, |
| TCM-Apo Ag | (Arbeitsgemeinschaft Deutscher TCM Apotheken): Anna Regina Flechtner, pharmacist, Alte Apotheke, Hauptstr. 12, 58739 Wickede, telefax 00-49-23-77-12-26, |
| University Witten/Herdecke |
Dr. Stefan Kirchhoff, TCM department, Witten/Herdecke University, Alfred-Herrhausen-Str. 50, 58448 Witten, telefax 00-49-23-02-92-67-07, |
Literature
- Melchart D, Linde K, Weidenhammer W et al: Liver enzyme elevations in patients treated with traditional Chinese Medicine. JAMA 282:1999, 28-29
- Al-Khafaji M: Monitoring of liver enzymes in patients on Chinese Medicine. J Chin Med; No.62:2000, 6-8
- Blackwell R. Adverse events involving certain Chinese herbal medicines and the response of the profession. J Chin Med No.50:1996, 12-22
- Vanherweghem J-L, Depierreux M, Tielemans C et al. Rapidly progressive interstitial renal fibrosis in young women: association with slimming regimen including Chinese herbs. Lancet 341:1993, 387-391
- Lord GM, Tagore R, Cook T et al. Nephropathy caused by Chinese herbs in the UK. Lancet 354:1999, 481-482
- Nortier JL, Martinez M-CM, Schmeiser HH et al. Urothelial carcinoma associated with the use of a Chinese herb (Aristolochia fangchi). NEJM 342:2000, 1686-92
- Wiebrecht A: Über die Aristolochia-Nephropathie. Dt Zschr Akupunktur 43:2000, 187-197
- Walb D, Krumme B: Nephropathie durch chinesische Heilkräuter. Arzneiverordnung in der Praxis 2001(2), 15
- Gundling K, Ernst E. Herbal medicines: Influences on blood coagulation. Perfusion 14:2001, 336-342
- Kirschbaum B. Atlas und Lehrbuch der Chinesischen Zungendiagnostik. Angewandte Zungendiagnostik - Differentialdiagnostik anhand von Fallstudien. Band 2. Verlag für Ganzheitliche Medizin Dr. Erich Wühr GmbH, Kötzting. 1. Auflage 2002, S. 265ff
- Ernst E. Adulteration of Chinese herbal medicines with synthetic drugs: a systematic review. J Intern Med 252:2002, 107-13
- Hong YS et.al: Large doses of Mutong cause renal failure. Zhejiang J Trad Chin Med 8:1965, 32
- Teschke R, Gaus W, Loew D. Kava extracts: safety and risks including rare hepatotoxicity. Phytomedicine 10(5):2003, 440-446